The future of prostate cancer diagnosis is right here, right now
/PSMA PET scanning shows multiple metastatic deposits of prostate cancer in lymph nodes.
Did you know that the way we diagnose prostate cancer in Australia is way ahead of the rest of the world?
Look up any clinical guidelines around the world and you’ll see that the standard process for diagnosing prostate cancer is to get a PSA (Prostate-Specific Antigen) blood test and if this is abnormal, to then undergo a random transrectal (via the rectum) prostate biopsy. There are so many reasons why this practice, still considered standard, is both archaic and barbaric. Allow me to explain.
First of all, an abnormally elevated PSA level can be due to 3 things: benign enlargement of the prostate, prostatitis, and prostate cancer. If we biopsy every man aged between 50 and 70 (the target age group for prostate cancer testing) with an elevated PSA, we know that about half will not have cancer. Their elevated PSA will be due to a benign condition. That's about 50% of men who are subjected to an invasive procedure unnecessarily. Why is that a problem? Because a standard transrectal prostate biopsy is dangerous, inaccurate, and often painful.
Transrectal prostate biopsy
In a transrectal biopsy, the biopsy needle is passed through the wall of the rectum numerous times to take samples of the adjacent prostate gland. As you might expect, the rectum contains an enormous number of faecal bacteria. These same bacteria are often injected by the biopsy needle directly into the prostate gland. It's OK for faecal bacteria to be in the rectum. That's where they belong. It's not OK for them to enter the prostate gland, which is normally sterile - there aren’t usually any bacteria in the prostate. When they do get in, they can cause acute bacterial prostatitis. Worse, because the prostate has such a rich blood supply, the same bacteria can then travel through the bloodstream, causing septicaemia. This is a life-threatening condition and we know that although exceedingly rare, men have died from prostate biopsy.
In an effort to reduce this risk, urologists have been routinely prescribing broad-spectrum antibiotics for patients who undergo a transrectal biopsy.
Now, bacteria are highly adept at developing resistance to these antibiotics. And they do it fast because, being single-celled organisms, they reproduce so rapidly. So the more we prescribe these broad-spectrum antibiotics, the more resistant these bacteria become. And that's exactly what is increasingly found in human rectums – highly antibiotic-resistant bacteria. So the typical preventative antibiotics that are being prescribed in transrectal biopsy are becoming less and less effective and the rates of septicaemia after transrectal biopsy are increasing around the world. That's why what should be a simple diagnostic procedure is actually dangerous.
It's also important to realise that when we perform a transrectal biopsy we have no idea where the cancer is - if indeed there is any cancer present at all. Even though we use ultrasound to guide the biopsy needle, this is simply to direct the needle into the prostate. It does not show us where cancer might be present within it. It is therefore essentially a blind biopsy. And that’s why this technique misses harmful prostate cancer up to 30% of the time.
Finally, depending on what type of anaesthetic is provided, transrectal biopsy is often painful.
So, if you were scheduled for a transrectal biopsy and you knew that there was a 50/50 chance that you don't even have cancer, and that if you do have cancer, there is a 30% chance of missing it, plus there is a 2% chance of septicaemia, plus you may find the procedure embarrassing, invasive and painful, would you still go ahead with it?
This is where the bad news ends and the good news begins. In Australia, this so-called “standard practice” is gradually being consigned to history.
MRI is a true game-changer in the diagnosis of prostate cancer and Australian urologists have been early adopters of it. Using a standardised method of MRI (multiparametric), for the first time we can reliably see the type of prostate cancer that has the potential to harm or even kill. Evidence is accumulating from other groups as well as ours telling us that getting an MRI should be the next step after finding an elevated PSA.
In stark contrast to a blind transrectal biopsy, a prostate MRI is safe, accurate, and painless. It's only real downsides: it can be claustrophobic, and currently there is no Medicare rebate (although we’re hopeful this will change soon), so it will set you back around AUD$400.
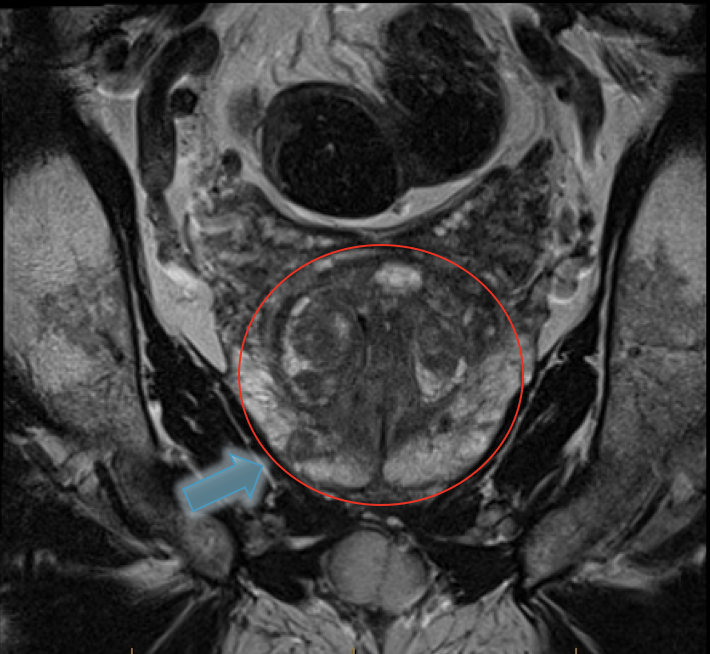
Multiparametric MRI of the prostate showing a cancer.
When performed after an elevated PSA, MRI can help us decide whether a biopsy is needed at all. If the MRI is clear, there is an excellent chance that there is no harmful prostate cancer present and a biopsy can be avoided. The other advantage is that if the MRI does show a suspicious lesion then the subsequent biopsy can target that lesion with high diagnostic accuracy. In summary, using MRI this way results in less unnecessary and invasive biopsies, but when a biopsy is needed, it is far more accurate. Win – win.
There is one very important condition however, and that is that the prostate MRI must be done properly to world standards and be reported by a radiologist who is highly experienced specifically in prostate MRI. Such experience remains relatively rare at present. For this reason, teaming up with the tech-savvy and entrepreneurial radiology trainee Dr Rowan Miller, we are currently building the world’s first online trainer to teach radiologists and urologists around the world how to read prostate MRI’s accurately.
But that's just the beginning of Australia's leading edge in prostate cancer diagnosis. We are also at the forefront of a safer method of prostate biopsy, when biopsy is truly required.
Transperineal biopsy - no needles in the rectum.
We have seen unprecedented uptake in performance of prostate biopsy via the skin – the so-called transperineal (via the perineum) biopsy. This method avoids the whole issue of resistant bacteria in the rectum as the biopsy needles are not passed through it. We have shown that the rate of infection is therefore zero or near-zero. And furthermore, there is no need for irresponsible use of broad-spectrum antibiotics, which in turn can promote further antibiotic-resistant bacteria. Another win – win situation!
But wait, there's more! Australia is yet again leading the way, this time with PSMA PET scanning (Prostate-Specific Membrane Antigen Positron Emission Tomography). Both a growing body of evidence, as well as our own clinical experience, tells us that PSMA PET scanning is far superior to traditional standard imaging for determining the extent of prostate cancer in a patient once cancer has been diagnosed.
Up till now we have been using both bone scans and CT scans for this purpose, knowing full well that unless there is obvious widespread disease, these two types of scans have a poor ability to detect metastatic (spread) prostate cancer. In other words, they are both poorly sensitive. In fact, they are also poorly specific, which means that when a suspicious lesion is found on these traditional types of imaging, it may not represent prostate cancer at all. Because of these deficiencies in traditional imaging, many patients have received inappropriate treatment for their prostate cancer.
PSMA PET scanning shows multiple metastatic deposits of prostate cancer in lymph nodes.
PSMA PET scan however provides us with far more accurate (sensitive and specific) information on which to base a treatment plan. Because this type of scan is so new, we do not yet have outcome data to confirm that these scans lead to improved patient outcomes. However, more accurate diagnostic information must surely point us in the direction of optimal management and risk minimisation.
These are truly exciting times to be a urologist working in this field in Australia. It is such a privilege and thrill to be able to offer our own patients not just world-class prostate cancer diagnostic tests, but world-leading prostate cancer diagnostics.